Actualités
-
3ᵉ Journée Scientifique du CRMR Spin@
Le CRMR Spin@ a le plaisir de vous annoncer sa 3ᵉ Journée Scientifique, qui se tiendra le Vendredi 5 juin 2026, de 9h à 17h30 Amphithéâtre Bilsky-Pasquier – Campus des Cordeliers – 15, rue de l’école de Médecine – 75006 Paris Cette journée sera l’occasion de réunir professionnels de santé, chercheurs, associations et partenaires autour […]
-
Signature de la Charte « Romain Jacob » : un engagement fort de l’hôpital Armand-Trousseau pour l’inclusion.
La Charte Romain Jacob, fruit du travail mené par Pascal Jacob, président de l’association Handidactique, est un engagement national visant…
-
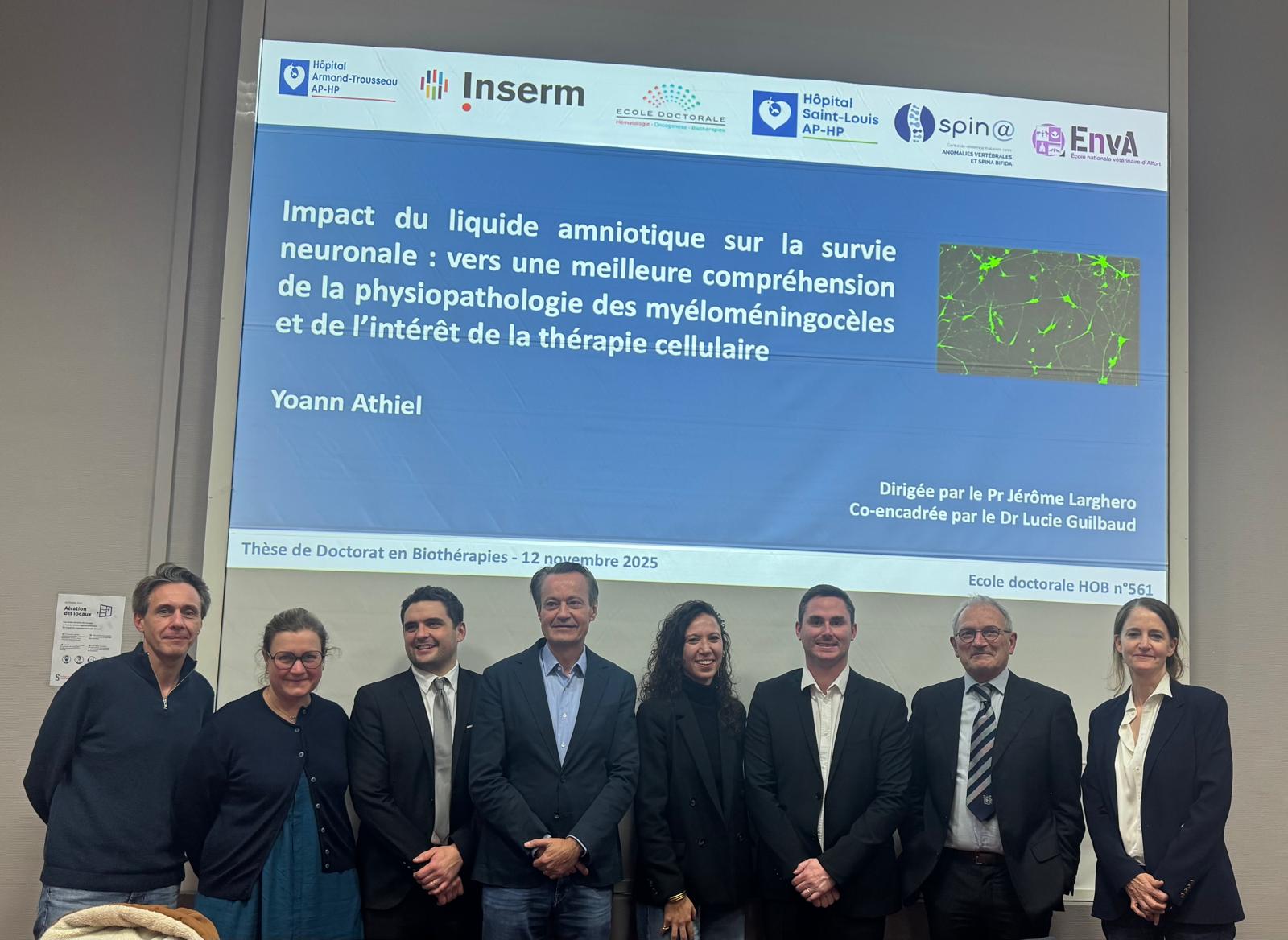
Soutenance de thèse : Dr Yoann Athiel
Le Dr Yoann Athiel est gynécologue-obstétricien et actuellement chef de clinique au sein du service de médecine fœtale de l’hôpital…
-
3ème Journée PRIUM : Mercredi 4 juin 2025
Le mercredi 4 juin, le centre coordonnateur Spin@ et en collaboration avec l’association de patients « Spina Bifida et Handicaps…
Nos publications
Dans: Fr J Urol, vol. 35, no. 13-14, p. 102938, 2025, ISSN: 2950-3930.
Pelvic organ prolapse is highly prevalent in women with spina bifida
Dans: BJUI Compass, vol. 6, no. 11, p. e70113, 2025, ISSN: 2688-4526.
Carte interactive
Retrouvez l’ensemble des centres constituant le CRMR Spin@ sur notre carte géographique interactive